Welcome
New this edition: Wise PBM Promo video, Current Medical Treatments and Medications for Plaque Psoriasis, Updates to Management of Clostridium Difficile, & MVI Flashpage Benchmark
Watch Our New
Promo Video
For Your Consideration
Current Medical Treatments and Medications for Plaque Psoriasis

You may have noticed that there has been a significant rise recently in the commercials touting the benefits of the newest generation of plaque psoriasis drugs. Our clinical line has also noticed a rise in calls related to these drugs, especially regarding cost. The following is a list of plaque psoriasis drugs along with approximate retail pricing per month.
Topical medications effective for psoriasis available by prescription include those that contain topical steroids of various potencies. Typical steroid medications are:
- Halcinonide (Halog, Halog-E) – $1200/2 60g tubes
- Flurandrenolide (Cordran, Cordran SP, Cordran Tape) – $915/120ml 0.05%
- Betamethasone(Luxiq) – $45/45g tube
- Desonide (Desonate) – $275/60g 0.05% tube
- Alclometasone (Aclovate) – $82/60g 0.05% tube
- Mometasone (Elocon) – $50/45g 0.1% tube
- Fluocinonide (Vanos) – $830/60g 0.1% tube
- Triamcinoloneacetonide (Kenalog) – $16/30g 0.1% tube
Tar-containing topicals and vitamin D-like molecules:
- Betamethasone/calcipotriene (Taclonex) $602/60g 0.005%-0.064% tube
- Calcipotriene (Dovonex) $435/60g 0.005% tube
Ultraviolet light administered under controlled conditions in a physician’s office in various wavelengths (narrow-band UVB) with or without supplemental medication (8-methoxypsoralen) (PUVA treatment) is a very effective therapy.
Systemic therapies include:
- Vitamin A-like drug, acitretin (Soriatane) – $569/25mg 30 capsules
- Short-term cyclosporine (Gengraf, Neoral, Sandimmune) therapy for severe flares – $218/25mg 60 capsules
- Methotrexate (Rheumatrex Dose Pack, Trexall) – $210/5mg 10 tablets
- Apremilast (Otezla) for mild to moderate psoriasis – $4350/30mg 60 tablets
The pricing on the biologicals vary depending on dosing schedule which can be a bit convoluted. One thing all of them have in common is that they are branded and very expensive.
The new targeted drugs called biologics, include:
- Etanercept (Enbrel) – $5172/month
- Adalimumab (Humira) – $5400/month
- Infliximab (Remicade) – $2800/month
- Ustekinumab (Stelara) – $2166/month
- Secukinumab (Cosentyx) – $5416/month
- Ixekizumab (Taltz) – $4200/80mg/ml syringe
- Risankizumab-Rzaa (Skyrizi) – $30,445/75mg/0.83ml 2 syringes
These products are produced by new technologies requiring their synthesis of living cells. They are proteins and all currently must be given by injection at various intervals into the subcutaneous tissue by the patient or by intravenous infusion in a medical facility. They are unique in that they have precise targets in the in the inflammatory pathway that they block. Since the biologics are very, very specific in their mode of action, they claim to offer increased safety and improved efficacy over older less specific immunosuppressive drugs.
All of these treatments must be continued indefinitely because when they are stopped, the psoriasis will typically return. It has recently been appreciated that the presence of psoriasis is a sign of a systemic inflammatory predisposition. Patients with psoriasis are predisposed to being obese, having diabetes, and having a destructive arthritis and premature cardiovascular disease.
For Your Consideration
Updates to Management of Clostridium Difficile
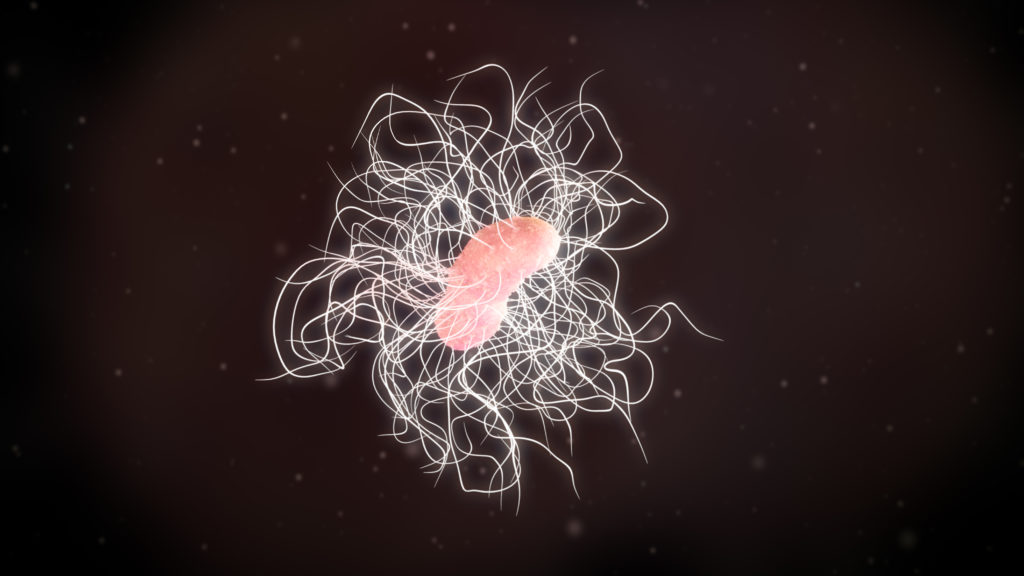
In February 2018, the Infectious Diseases Society of America (IDSA) and the Society for Healthcare Epidemiology of America (SHEA) released an update in the clinical practice guidelines for CDI in adults and children, which included new recommendations. The biggest change from the previous guideline involves the initial treatment of CDI.
The CDC estimates that C difficile affects a half-million people each year, and 20% of those affected may become infected again. It is reported that 1 in 11 people over the age of 65 years died of a healthcare-associated C difficile infection (CDI) within a month of diagnosis. Risk factors for C difficile include antibiotic use, age older than 65 years, recent hospitalizations, a weakened immune system, and previous CDI or known exposure. The highest risk of CDI occurs during and in the first month after antibiotic exposure. Extended antibiotic use and use of multiple antibiotics further increase the risk of CDI. Chemotherapy, gastrointestinal surgery, and use of acid-suppressing medications like proton pump inhibitors or histamine-2 blockers are risk factors as well.
Metronidazole is no longer recommended as first-line therapy for adults. Oral vancomycin and fidaxomicin are now supported as first-line options for both non-severe and severe initial episodes of CDI. This change stems from evidence that either option ensures resolution of symptoms and sustained resolution one month after treatment. Metronidazole is only recommended for nonsevere initial episodes when patients are unable to obtain or be treated with oral vancomycin or fidaxomicin.
Approximate Retail Pricing:
• Vancomycin (oral) 125mg 4x daily for 10days = $600
• Fidaxomicin/Dificid (oral) 200mg 2x daily for 10 days = $3900
As stated above, metronidazole is used when vancomycin or fidaxomicin are unavailable. Vancomycin and fidaxomicin have a better cure rate than metronidazole but, in our opinion metronidazole may be prudent as first-line treatment for CDI symptom management based upon where an individual is in their disease trajectory and their overall prognosis.
• Metronidazole (oral) 500mg tid x10 days = $40
For the complete article by Kimberly E. Ng, PharmD, BCPS follow this link
https://www.medscape.com/viewarticle/913901_1
| Clinical Definition | Supportive Clinical Data | Recommended Treatment for C. Diff |
|---|---|---|
| Initial episode, nonsevere | Leukocytosis with a white blood cell count of <15,000 cells/mL and a serum creatinine level <1.5 mg/dL |
|
| Initial episode, severe | Leukocytosis with a white blood cell count of ≥15,000 cells/mL and a serum creatinine level >1.5 mg/dL |
|
| Initial episode, fulminant | Hypotension or shock, ileus, megacolon |
|
| First recurrence |
|
|
| Second or subsequent recurrence |
|
Treatment recommendations from the 2018 Guidlines
Performance Update
Latest MVI Flashpage Benchmarks WHO As Lowest Cost PPD PBM

About Multi-View Inc
Perhaps no other organization has meticulously considered and cared enough about the Hospice, Homecare and post-acute experience to breakdown and systematize everything from phone interactions to clinical visits to revolutionary bereavement to enormous utilization of volunteers to the economic welfare of the mission.
After working with over 1,000 healthcare entities, MVI starts with Benchmarking for professional perspective and guides an organization all the way through the Model with its establishment of 1) Clear, 2) Impressive and 3) Sustainable Standards. Then via extraordinary People Development, an organization with near-flawless quality is created, where it can go days, sometimes weeks, and even “thousands of visits or interactions” between complaints, service failures or documentation errors.
Economic results are often 200-300% above average and are a natural byproduct of radically increased quality.
Wise October 2019 Flashpage Benchmarks
- Pharmacy NPR%* – 4.0%
- Pharmacy PPD – $6.26
- Patient-Related NPR% – 16.6%
- Net Op. Income NPR% – 16.6%
- RN Average Visit Duration – 1:09
*Percentage of net patient revenue
The numbers listed above represent a median reported by our Hospice clients participating within the MVI program.
For a more detailed analysis and comparison to competitors please reach out to MVI for a subscription to their services.
Wise Clinical Team

Deanna Rice
Vice President Clinical Services
drice@wiseop.com
(800) 856-9757 – EXT. 216

Tino Vilches
Senior vice president clinical services
tvilches@wiseop.com
(800) 856-9757 – EXT. 208
David Bougher
Senior VP of Regulatory Affairs
dbougher@wiseop.com
(800) 856-9757 – EXT. 203
Available
Wise Hospice Options Services
24/7 Support
On-demand clinical or technical assistance fast.
EHR Interface Integrations
Demographic & medication interfaces with over 10 EHR's.
E-Prescribing
Web-based prescribing platform for Schedule II's.
Pharmacy Network Access
Unrestricted access to every pharmacy within our network.
Advanced Reporting
Drill down into your pharmacy utilization trends.
Clinical Education
Hospice oreiented courses designed for your hospice staff.
EHR Medication Profiling
Med reviews done inside your EHR system within 5 days.
Formulary Management
Develop a performance based formulary with our clinical team.
Web-based Refills
Send and identify available refills for your patient population.







